What is Spinal Stenosis?
Spinal stenosis is a common cause of back pain. What is spinal stenosis? What causes it? And how do you diagnose and treat it?
I recently received the following inquisitive email from an eager listener:
“Is it possible to make a post about things like…spinal stenosis and any other bone related issues? I have spinal stenosis…,[and] stress in general, so with sudden pains in places I don’t identify with stenosis, I panic and rush to the ER and obviously cannot run to the ER with every quirk I get…so to have info on issues of the bones would be of much help…probably to others as well? Thanking you in advance if you will make a thread about what I’m asking.” ~ A.P.
Thanks A.P. for your topic suggestion. And indeed, spinal stenosis is quite a common physiological condition. And back pain is the fifth most common reason that drives people to the doctor’s office. Most of the time, back pain is self-resolving and benign. However, there are rare causes of back pain that can be emergent, and I’ve reviewed these red flags and how to prepare for your back pain visit in a prior article, along with the common causes and treatment options of low back pain in a subsequent article.
But let’s tackle spinal stenosis specifically today. Spinal stenosis is not often an emergency. It may become chronic and is sometimes a progressive condition of the back, but it’s not usually a reason people need to dart to the ER. Let’s review what spinal stenosis is, the symptoms, and some treatment options.
The Anatomy of the Spine
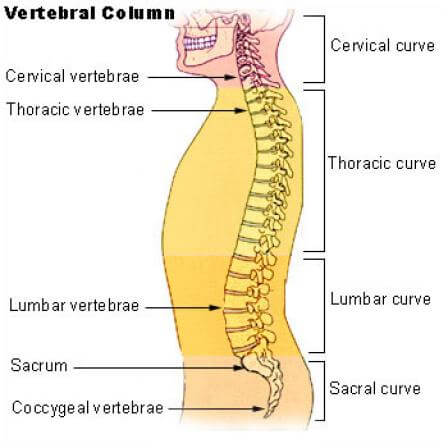
The spine originates in the back of the skull and spans all the way down into the pelvis, and is made up of smaller blocks called “vertebrae” (think LEGOS). There are five different types of these LEGO vertebrae regions:
- The cervical spine (or C-spine for short) includes seven vertebrates and runs from the back of the head and extends through the neck.
- The thoracic spine (T-spine) houses 12 vertebrates that span the upper to mid-back.
- The lumbar spine (yep, you guessed it, the L-spine) consists of five vertebrates that encompass the lower back, the most commonly injured region of the spine.
- The sacral spine (this one is simply referred to as the “sacrum”) contains five vertebrates as well, but they are fused and therefore appear smoother. The non-medical term often used for the sacrum and beyond is the “tailbone.”
- The coccyx is the very tip of the spine and includes anywhere from three to five also-fused vertebrate.
Here’s a helpful image to visualize this anatomy.
Within the spinal cord lies a long canal that spans from the C-spine and ends at the first lumbar vertebrate. This canal houses the numerous nerves that run down the spine and exit at various levels to feed your body parts. The spinal cord ends at the first lumbar vertebrate, but the nerves still continue on past that and through to the tailbone.
Directly in front of the spinal cord lies a thick, roundish ring with a central jelly-like fluid within the spine. This is the “disk” that is referred to in “herniated disks.” It is there to help cushion the spinal cord in the canal, and to prevent all the little bones of the spine from rubbing against each other.
What is Spinal Stenosis?
The word “stenosis” denotes a compression, and in spinal stenosis it refers to a spinal canal that is compressed by the nearby surrounding structures that impinge on the nerves running through the canal. Therefore, if the nerves have less room, they can become aggravated and can cause what’s called neurologic compromise. If the stenosis is at the C-spine, then it will affect the nerves that run down the arms. And if the stenosis is at the lumbar spine, then it can impinge upon the nerves that run down the legs.
What Causes Spinal Stenosis?
What causes that canal to become stenotic, you may be wondering? Well, this is the root of it all (no pun intended). People can be born that way (referred to as “congenital” spinal stenosis) or it can develop through time and age.
- Arthritis is the most common cause. The vertebrate and its bony structures can wear and tear through time. And this arthritic degeneration can impinge on the nerves within the canal and cause spinal stenosis.
- Herniated disks can also cause spinal stenosis, by protruding and encroaching on the spinal nerves that it’s supposed to be cushioning and protecting. Herniated disks are common. Many of us may have one (or more) without knowing, because it doesn’t always cause pain. It’s overall benign, unless it chronically affects the nerves it compresses.
- Spondylolisthesis is another potential cause of spinal stenosis (no, you don’t have to know this word or even say it out loud). It refers to when a vertebrate is out of alignment with the rest of the adjacent vertebraes. If it slips too far forward, it can place pressure on the nerves inside the canal. Check out this image from the American Academy of Orthopedic Surgeons.
- Tumors near or in the spine can also compress the canal. Many of these tumors may be benign, such as lipomas or cysts, but are an infrequent cause of spinal stenosis.
- Lastly, bone disease can affect the bones of the spine. Examples include autoimmune disorders such as rheumatoid arthritis or ankylosing spondylitis. These conditions are often hereditary.
Symptoms of Spinal Stenosis
Now that we have learned the root of the condition, let’s review some of the more common symptoms that spinal stenosis induces.
First of all, many people with spinal stenosis have no symptoms at all. Or their symptoms may be mild, transient, and self-resolving.
Because the nerves are encroached upon, the symptoms of spinal stenosis may include the nerves. Numbness and tingling in the legs or feet in lumbar stenosis, or hands or arms in cervical stenosis reflect nerve involvement.
Back pain is also a potential symptom. Pain is usually induced by certain activity, such as standing, walking, moving a certain way, etc. Most people tell me they don’t have pain at rest and leaning forward provides relief in some.
Bed rest can worsen symptoms and is not typically recommended for those with spinal stenosis or back pain.
If spinal stenosis symptoms become chronic, however, they will chronically injure the nerves as well. And people may experience weakness of the legs or arms eventually. Doctors would like to avoid this from happening to patients, and if the symptoms become chronic they may require further care from a specialist.
Diagnosis and Treatment of Spinal Stenosis
Spinal stenosis can often be seen on an X-ray. An MRI is not typically necessary and is a costly test without further usefulness most of the time (unless the patient is a surgery candidate or the pain becomes chronic).
And its treatment is conservative. That means we often treat it the same as other causes of back pain, such as muscle strains, herniated disks, arthritis, etc. This includes medications to calm down the inflammation, muscle relaxants, physical therapy, ice or heat, and sometimes steroid injections. I’ve reviewed treatment of low back pain in detail prior, so review my previous episode if you’d like more specifics.
If spinal stenosis is severe, sometimes surgery is recommended in order to save the limbs from weakness or chronic nerve damage. Like most elective surgery, it is often a last resort.
Whatever you do, stay active. Bed rest can worsen symptoms and is not typically recommended for those with spinal stenosis or back pain.
Back Pain Red Flags
There are certain instances in which back pain becomes urgent and sometimes a dire emergency. If you have any of the following, please see your doctor right away:
- Trauma that precipitated the pain.
- Urine or bowel difficulties.
- Numbness or changes in sensation of the genitals or buttocks.
- Motor deficits (weakness of the limbs).
- Fever.
- Unintentional weight loss.
- History of cancer.
- If the pain is so severe that you cannot find a comfortable position.
Share your ideas and learn more quick and dirty tips with us on the House Call Doctor’s Facebook, Twitter, and Pinterest pages! If you learned anything here today, or simply enjoy all-things-medical, you can also listen and subscribe to the House Call Doctor podcast on Apple Podcasts, Spotify, and Stitcher.
Please note that all content here is strictly for informational purposes only. This content does not substitute any medical advice, and does not replace any medical judgment or reasoning by your own personal health provider. Please always seek a licensed physician in your area regarding all health related questions and issues.
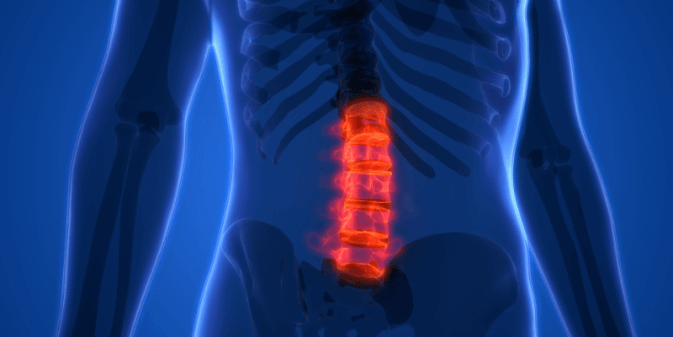
Image of a spinal cord © Shutterstock